Happy&Healthy, Health Talk FM.102 every Saturday 9:00–10:00 a.m.: Sleep Apnea
Happy&Healthy, Health Talk FM.102 every Saturday 9:00–10:00 a.m.: Sleep Apnea
Sleep Apnea
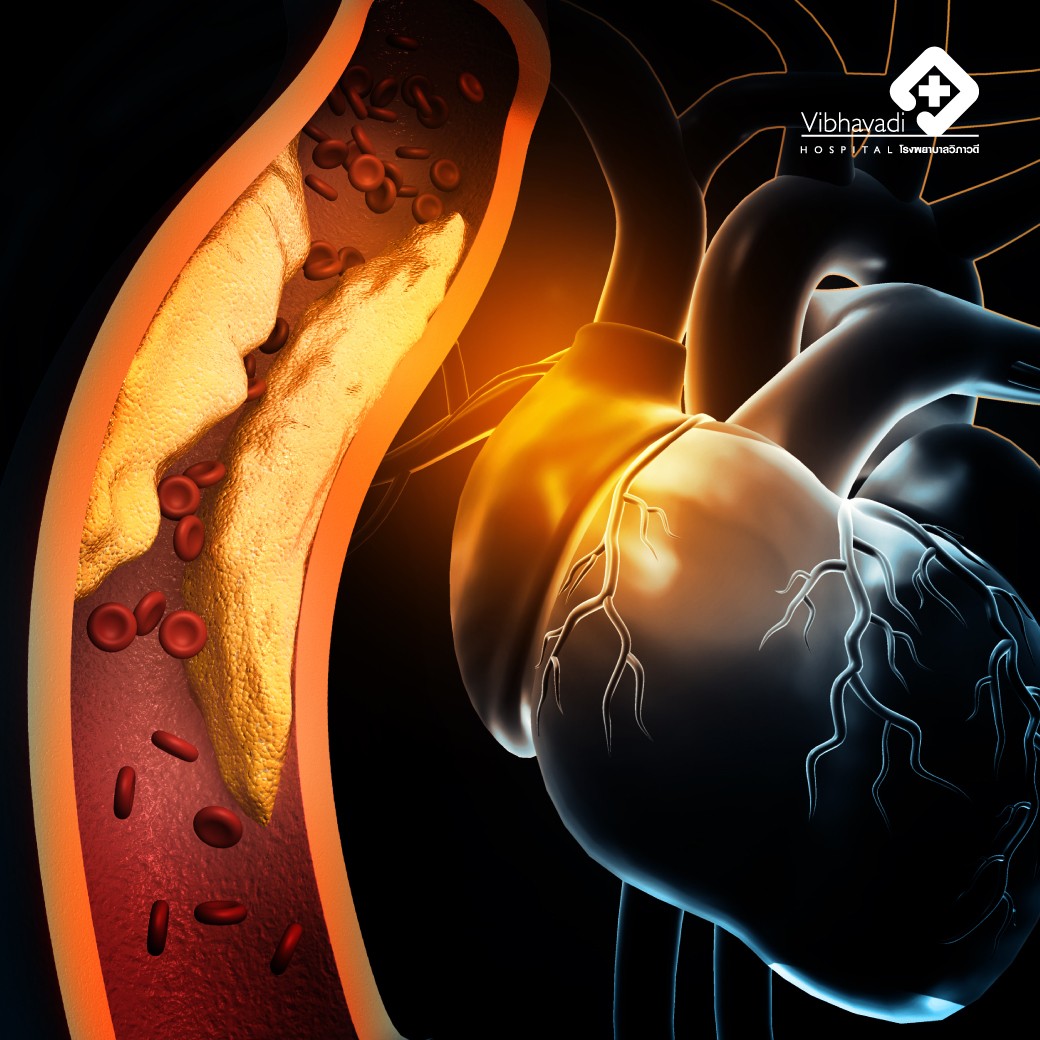
Snoring is a symptom that can affect individuals of all genders and ages, and it is important to recognize it as an early warning sign of potential health risks. It can have various negative impacts on our well-being, such as morning headaches and excessive daytime sleepiness. Prolonged and loud snoring can even have adverse effects on the brain and heart. It increases the risk of developing conditions like sleep apnea, high blood pressure, coronary heart disease, and cerebrovascular diseases, including stroke and paralysis.
Obstructive sleep apnea is a specific type of sleep disorder characterized by the narrowing of the airway passages. This narrowing leads to breathing difficulties, including shallow breathing or complete cessation of breathing. When breathing stops, the oxygen levels in the blood decrease, impacting the functioning of other organs in the body.
Sleep apnea commonly occurs in individuals with excessive tissue in the neck or sagging tissue that narrows the airway. Certain risk groups are more prone to this condition, including overweight individuals, those with abnormal facial structures like small jaws, older adults with brain diseases or muscle weakness, individuals who consume alcohol or use sleep-inducing medications like benzodiazepines. Men are often at higher risk than women, although women post-menopause can experience a resurgence of risk due to changes in muscle tightness. Additionally, individuals with cerebrovascular diseases or heart conditions may experience sagging of the pharyngeal muscles or thickening of tissues around the neck, further narrowing the airways.
Symptoms that indicate the presence of sleep apnea include:
1. Loud snoring.
2. Interruptions in snoring followed by complete silence, or occasional abrupt awakenings due to gasping or choking for air.
3. Frequent headaches upon waking.
4. Feeling unrefreshed after sleep, as if not having had a restful night.
5. Experiencing a sore throat or dry throat upon awakening.
6. Excessive daytime sleepiness, often leading to unintentional napping in inappropriate situations, such as while driving.
7. Individuals with poorly controlled underlying conditions, such as high blood pressure, may require at least three types of blood pressure medication.
If left untreated, sleep apnea can have direct impacts on the brain and cardiovascular system. In the initial stages, it can lead to persistent daytime sleepiness, decreased concentration, mood changes, irritability, or even depression. In older individuals, it can contribute to the development of dementia. The effects on the heart and blood vessels occur during episodes of respiratory arrest, where the body experiences a lack of air. As a compensatory response, the heart works harder and faster, leading to potential complications such as irregular heartbeat, heart attack, arterial hardening, high blood pressure, or cardiovascular diseases like myocardial infarction and cerebrovascular diseases, including paralysis.
Diagnosing sleep apnea involves a comprehensive approach that includes obtaining a detailed medical history, conducting a thorough physical examination, and performing sleep monitoring tests, such as polysomnography or sleep tests. These tests help assess the severity of the condition and guide treatment recommendations. During sleep examinations, devices are used to monitor various bodily changes, including brain waves, oxygen levels, heart waves, and muscle activity. Before undergoing the examination, patients are advised to abstain from stimulants like tea, coffee, cocoa, or other substances that can disrupt sleep, as well as certain medications that may affect sleep.
The severity of sleep apnea is typically determined by the Apnea-Hypopnea Index (AHI), which measures the number of breathing interruptions per hour. AHI values ranging from approximately 5 to 15 are considered mild, while 15 to 30 are classified as moderate. AHI values exceeding 30 are considered severe, requiring immediate treatment due to the potential negative long-term effects associated with the condition.
Treatment
1. Continuous Positive Airway Pressure (CPAP): This is the primary and most effective treatment for sleep apnea. It involves wearing a mask connected to a machine that delivers a continuous flow of air pressure to keep the airway open while sleeping. CPAP helps prevent breathing interruptions, fainting, and snoring.
2. Dental devices: These are custom-made oral appliances that are fitted by dentists. The dentist will assess if there are any contraindications, such as jaw joint disease or suitability based on the number of teeth. These devices work by keeping the airway open during sleep and are only worn while sleeping.
3. Surgical interventions: Surgical options are considered when CPAP and dental devices are ineffective or not suitable for the individual. An otolaryngologist specializing in sleep disorders will evaluate the underlying cause of airway narrowing. For example, in some cases, the tonsils may be removed, or excess tissue behind the uvula and soft palate may be corrected. The decision to pursue surgical intervention is made on a case-by-case basis.
To prevent the disease, it is important to maintain a healthy weight and avoid becoming overweight. It is also essential to treat any nasal diseases, such as nasal allergies, rhinitis, or deviated nasal wall, to prevent narrowing of the airway in the future. Avoiding alcohol consumption is also recommended as it can cause the muscles to relax. Smoking can cause swelling of the nasal mucosa and should be avoided. Individuals using benzodiazepine sleeping pills should consult a sleep doctor to adjust their medication to prevent the occurrence of obstructive sleep apnea. Additionally, allowing excessive weight gain can increase the risk of developing obstructive sleep apnea and other related diseases. Therefore, if an individual or their spouse and child snore loudly on a regular basis, they should visit a doctor for advice and appropriate treatment.
by Dr. Pongsakorn Tanayapong, Neurological Pathologist